Design and Additive Manufacturing Processes of Oral Maxillofacial Patient-specific Reconstructive Surgery

Onur Demirak
Medical Application Engineer
In case of severe bone atrophy and edentulism, traditional dental implants can only provide inaccurate treatment periods leading excessive ridge resorption eventually. About 80 years ago, subperiosteal cast frameworks have been developed using analogue radiographical imaging, however, they led to imprecise designs and implant failures caused by stress shielding effect.
Additively manufactured subperiosteal jaw implants (AMSJIs) has been demonstrated in 2017 to lay down alternative approach. This study aimed to explain TraBtech’s workflow to generate innovative designs with biomimetic purposes for subperiosteal frames and fabrication of them by using powder-based additive manufacturing.
The development process, in brief, begins with radiological data acquisition and 3D anatomical remodelling. The implant design is made according to a 3D anatomical model. After finite element methods are applied, the implant is produced by using selective laser melting.
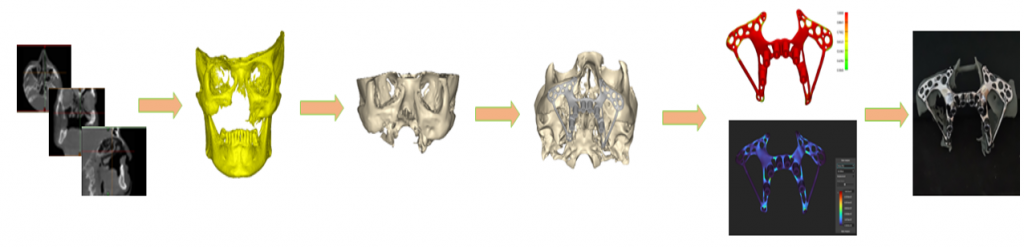
Figure 1: Flow of the study
3D Anatomical Modelling
There are various data types used for reconstruction from 2D images to 3D models. Specific to the oral maxillofacial region, CT and CBCT are both used to 3D reconstruct the model for different design approaches. We preferred CT with .5 mm slice thickness in this case.
After the determination of the scope of the study inventorial path should be built. There are a good many computer-aided design, engineering and manufacturing software present which is used in the medical field as tools for digital surgical planning, implant designing, analyzing, and pre-fabrication planning.
Custom-made implant design flow has one of the most crowded inventory lists which includes almost everything I mentioned. In this study we use Mimics Innovation Suite software which is formed by the programs specialized in this flow to eliminate the risk factor between data transfer and to follow a validated medical procedure.
Image processing algorithms are used to segment, and characterize the specific anatomic region to obtain accurate 3D models. In some cases of different radiological data is preferred, anatomical re-modeling can be needed. It requires both engineering and radiology knowledge to create “Digital assumptions” on the anatomical surface which will be used for further steps. Even we have capability to remodel the bone tissue with Mimics, we didn’t need for such a step in this study, because of using a proper resolution of CT.
The oral MAXF region of the patient has been modeled, and the surgical steps are figured out via a digital and physical medical model.

Figure 2: Medical Image Processing
Implant Development
Implant design is made by using medically verified software. Contours, thicknesses, geometry, fixation points and abutment locations are determined according to analyze results and outcome of engineer-physician collaboration. Topology optimization concept has been implied as a mathematical method that optimizes material layout for a given loads, boundary conditions and constraints with the goal of maximizing the performance while minimizing materials, thus costs.
The design approach must be constructed according to the limitations of the chosen additive manufacturing technology, in other sayings, design for additive manufacturing (dfAM) rules must be adopted to all steps of 3D modeling. The chosen material also affects the design approach by the reason of the mechanical behavior while printing.

Figure 3: 3D Anatomical Design and Structural Analysis
After topology optimization of the subperiosteal frame, fixation point locations were determined by using maxillary Wall thickness analysis. The preferred screw was transferred to the digital platform with its critical properties such as length and Radius by reverse engineering approach. The surgeon has been guided by a roadmap including analysis results. In this study, minimum 5 mm of bone thickness has been desired for fixation locations.
Abutments can be designed in various ways according to the clinical aim and preferred dental suprastructure as you can see in the figure. Vertical distances were decided based on to the wax trial which also can be expressed as a 3D model from CT source.
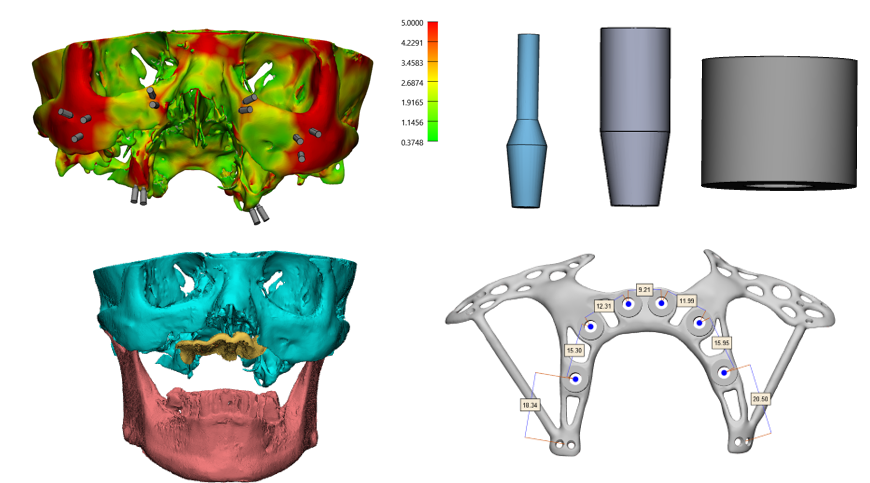
Figure 4: Maxillary Wall Thickness Analysis, Abutment Types and Abutment Planning
Additive Manufacturing
Additive manufacturing (AM) has a huge raw material pool and the determination of the material of the implant located in the oral MAXF region depends on 3 main aspects:
1.Mechanical behavior of the material and its relevance with the anatomical region implanted
2.Biological requirements of the region
3.Producibility of the material via determined additive manufacturing technology
As it would be appreciated, not every material is available to fabricate by any technology. For AMSJI we used Titanium Alluminium Vanadium Grade 23 alloy due to its high strength, low weight, and excellent corrosion resistance. Also, the material must be medically verified by completing the mechanical and biological tests to make it commercially available as additive manufacturing raw material.
This metal alloy has been fabricated with selective laser melting Additive manufacturing technique. This technique uses a powder bed with a heat source to create metal parts layer by layer.
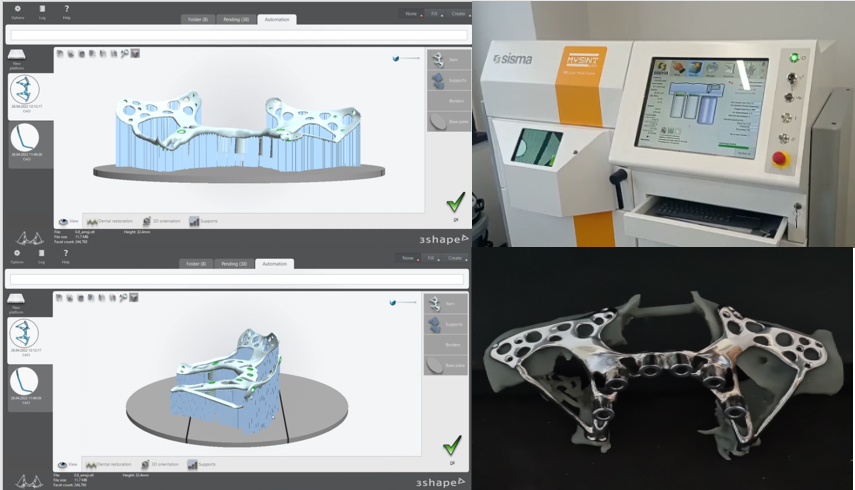
Figure 5: Pre-Fabrication Planning and Additive Manufacturing
To sum things up the patient-specific implants are developed especially for exceptional cases where the standard implant solutions are insufficient. There are many steps to obtain an accurate patient-specific implant, and it requires expertise in medical and engineering sciences and validated process elements. The development process of the patient-specific implants begins with data acquisition. Radiological image source formats are usually CT or CBCT for the oral and maxillofacial area. Then, these 2D images are reconstructed as precise 3D models via medical image processing. 3D digital models can be converted to physical models via 3D printing to plan the surgery at this point. The implant design and fabrication practice consist of 3D modeling, analysis, and additive manufacturing (AM). Medically certified software, materials, and machines must be utilized for all stages. The implant is 3D modeled as a result of engineer-physician collaboration. It is aimed to design and produce implants fully adaptable to the irregular bone structure of the region, topologically optimized-reduced weight, and cost according to structural analysis results. The material and AM methods are chosen according to the needs of mechanical and biological performances and producibility.

This article is a compilation of the presentation made at AÇBİD 15th International Congress with special thanks to authors, Aydın Onur Gerçek, Hakan Hıfzı Tüz, Emre Tosun and Faculty of Dentistry, Hacettepe University, Ankara, Turkey